What Is Rheumatoid Arthritis? Symptoms, Causes & Treatment

Rheumatoid Arthritis is a complex autoimmune disease that can be overwhelming. understanding this condition is crucial for those diagnosed and their loved ones. It's necessary to understand what comprises this condition and the potential threats that can come along. It is also vital to keep track of the details of this condition to be aware of when to seek medical help before it's too late. Lets review Rheumatoid Arthritis and get a hang of this illness.
Understanding Rheumatoid Arthritis
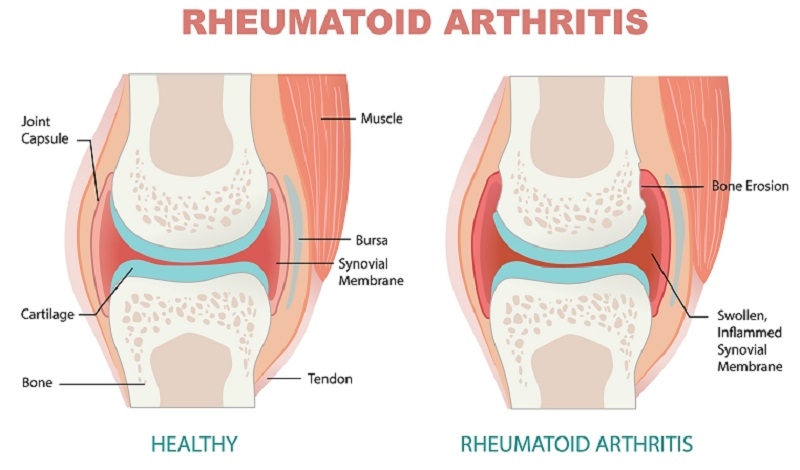
Arthritis is an autoimmune disorder in which the body's immune system mistakenly attacks the synovium, the lining of membranes surrounding the joints. Unlike osteoarthritis, which results from wear and tear on the joints, RA is characterized by chronic inflammation, leading to joint pain, stiffness, and damage over time. The exact cause of RA remains unknown, but it's believed to involve a combination of genetic, environmental, and hormonal factors.
Types of Rheumatoid Arthritis
Seropositive Rheumatoid Arthritis:
Seropositive RA is characterized by specific antibodies in the blood, namely rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies. These antibodies are typically elevated in the blood of individuals with this type of RA.
Seropositive RA often presents with more severe joint inflammation and damage than seronegative RA. It may progress more rapidly, and joint deformities are more common. This type of RA tends to be associated with a more active and aggressive disease course. Individuals with seropositive RA may require more intensive therapy to control inflammation and prevent joint damage.
Seronegative Rheumatoid Arthritis:
Seronegative RA refers to cases of RA where the specific antibodies rheumatoid factor (RF) and anti-CCP are not detected in the blood. Despite the absence of these antibodies, individuals with seronegative RA still experience RA symptoms and joint inflammation. Seronegative RA tends to have a more variable and unpredictable course.
In some cases, it is less aggressive than seropositive RA, but it can still lead to significant joint damage and disability. Joint involvement and symptom severity can vary widely among individuals with seronegative RA. The absence of these antibodies does not necessarily indicate a milder form of RA. Diagnosing seronegative RA may be more challenging due to the lack of specific markers in the blood.
Rheumatoid Arthritis Symptoms
RA manifests in various ways, and symptoms can vary from person to person. However, some common signs and characteristics include:
- Joint pain often occurs on both sides of the body.
- Joint stiffness, especially in the morning or after inactivity.
- Joint swelling and tenderness.
- Overwhelming Fatigue
- Systemic symptoms include fever, weight loss, and muscle weakness.
- Joint deformities and loss of function as the condition progresses.
Causes/Risk Factors of Rheumatoid Arthritis
While the exact cause of RA remains elusive, several risk factors have been identified:
- Genetic predisposition: People with a family history of RA are at an increased risk.
- Gender: RA is more common in women than in men.
- Environmental factors: Smoking, exposure to certain infections, and other environmental factors may contribute to RA development.
- Hormonal factors: Hormonal changes, such as those occurring during pregnancy, can influence the onset and severity of RA.
Diagnosis of Rheumatoid Arthritis
Diagnosing RA involves a combination of clinical evaluation, laboratory tests, and imaging studies:
- Clinical evaluation: A rheumatologist will assess your medical history and perform a physical examination to check for joint tenderness, swelling, and range of motion.
- Blood tests: These may include rheumatoid factor and anti-CCP antibody tests to identify specific markers of inflammation.
- Imaging tests: X-rays, ultrasound, and magnetic resonance imaging (MRI) can reveal joint damage and help track disease progression.
Treatment for Rheumatoid Arthritis
Managing RA effectively requires a comprehensive approach tailored to each patient's needs. Treatment options include:
Physical Therapy:
Physical therapists design exercise programs to improve joint mobility, muscle strength, and overall physical function. They can also teach patients techniques to protect their joints during daily activities. Occupational therapists assist patients in adapting their environments and routines to minimize stress on affected joints.
Lifestyle Modifications:
- Rest and pacing activities: Adequate rest and moderation help manage fatigue and prevent joint strain.
- Exercise: Regular, low-impact activities like swimming, cycling, and gentle stretching can help maintain joint flexibility and muscle strength.
- Stress management: Stress can exacerbate RA symptoms. Techniques like relaxation, mindfulness, and stress reduction strategies can be beneficial.
Surgical Interventions:
- Joint Replacement: In cases of severe joint damage and disability, joint replacement surgery (arthroplasty) may be recommended. Commonly replaced joints include the knees, hips, and shoulders.
- Synovectomy: This procedure involves the removal of the inflamed synovial tissue that lines the joints and can help alleviate pain and reduce joint swelling.
Assistive Devices:
Orthopedic aids like splints, braces, and shoe inserts can provide support and reduce joint stress. Mobility aids such as canes, walkers, or wheelchairs may be necessary for individuals with significant joint damage.
Medication Management:
Regular monitoring and adjustments of medication doses are essential to ensure optimal disease control while minimizing side effects. Rheumatologists work closely with patients to assess treatment responses and make necessary modifications.
Rheumatoid Arthritis Medications
Medications play a pivotal role in managing RA. Let's delve deeper into the categories of drugs used:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These drugs, including ibuprofen and naproxen, help reduce pain and inflammation. They are typically used to provide symptomatic relief.
- Disease-modifying antirheumatic drugs (DMARDs): DMARDs are essential for slowing the progression of RA. Methotrexate is a commonly prescribed DMARD that has proven effective in many cases.
- Biologic DMARDs: These medications target specific immune system components responsible for inflammation. Biologics like etanercept and adalimumab have shown promise in managing RA.
- Corticosteroids: Prednisone and other corticosteroids can provide rapid relief from RA symptoms but are generally used for short-term management due to potential side effects.
The choice of medication depends on the severity of the disease, individual response, and the patient's overall health. Your rheumatologist will work with you to determine the most suitable treatment plan.
Rheumatoid Arthritis Diet
While diet alone cannot cure RA, confident dietary choices may help manage symptoms and promote overall well-being:
- Omega-3 fatty acids: Found in fatty fish like salmon and walnuts, these healthy fats may have anti-inflammatory properties.
- Antioxidant-rich foods: Fruits and vegetables, especially those with vibrant colors, are high in antioxidants, which can help combat inflammation.
- Limit processed foods: Processed and high-sugar foods may exacerbate inflammation. It's best to reduce their intake.
- Stay hydrated: Proper hydration can help maintain joint function and reduce stiffness.
- Consider dietary supplements: Some RA patients may benefit from vitamin D and calcium supplements to support bone health.
It's essential to consult with a healthcare provider or registered dietitian before making significant dietary changes, as individual needs and sensitivities vary.
Learn about: Osteoarthritis: Causes and Proven Treatments
Conclusion
Rheumatoid Arthritis is a complex and challenging condition, but with proper understanding and management, individuals living with RA can lead fulfilling lives. Early diagnosis, appropriate medical treatment, physical therapy, and lifestyle adjustments are essential for better disease control. While there is no one-size-fits-all solution for RA, ongoing research and advancements in treatment options offer hope for improved outcomes and a brighter future for those affected by this autoimmune disorder.
This content was created by AI
-1717753922-r.jpg)